Mohamed Lachemi details how the university is monitoring the outbreak

Ryerson president Mohamed Lachemi says the university has systems in place to monitor any new developments in the coronavirus spread.
On Monday, Lachemi responded to concerns about COVID-19 in a meeting with the Ryersonian.
“If any community member is planning upcoming travelling, especially dealing with the business of the university, we want them to notify us and then be in touch with [Ryerson’s Office of International Affairs],” said Lachemi. “It’s important for us to talk with them.”
Lachemi said the university’s Office of International Affairs is monitoring the situation on a daily basis. “[We] are also looking at what’s happening at other locations and would make a case-by-case determination related to upcoming university-related travel,” he added.
Lachemi said Ryerson works “very closely” with public health agencies such as the Ontario Ministry of Health and Long-Term Care, Public Health Ontario and the Public Health Agency of Canada. He also said Ryerson continues to gain knowledge from other agencies, including a network of Ontario universities, to share information and good practices.
“We have actually a committee called the public health committee that meets on a weekly basis to determine precautions or action on the advice of public health,” said Lachemi.
Along with that committee, Ryerson also has an emergency management team “that would mobilize to consider the continuity in an event on campus,” Lachemi added.
What are coronaviruses?
The disease that has been spreading and was first labelled “novel coronavirus” is called COVID-19 by the World Health Organization (WHO). The virus that causes this disease is called SARS-CoV-2. To avoid causing unnecessary panic, the WHO refers to the virus as that which is “responsible for COVID-19.”
Previous coronaviruses include MERS and SARS. According to a recent study, coronaviruses account for 10 to 30 per cent of respiratory tract diseases in adults. When infected with a coronavirus, a person may face symptoms similar to those of the common cold. But in severe cases, coronaviruses can cause intestinal and neurological disease. The incubation period, the time frame until the symptoms of a coronavirus manifest, can be two weeks or longer.
When COVID-19 infects the respiratory tract, common symptoms like fever and dry cough emerge. Severe outcomes include pneumonia, kidney failure and possibly death.
MERS and SARS were spread through coughing and sneezing. Given COVID-19 can be spread like MERS and SARS, similar prevention measures are used. WHO suggests wearing a mask if you are in contact with a person infected by COVID-19, and using a disinfectant to clean your hands.
Origin of COVID-19
The virus was first detected in Wuhan, a city in China’s Hubei province with a population of 11 million. The virus was recognized after a pneumonia outbreak without a certain cause, and while the majority of infection and deaths have taken place in China, COVID-19 quickly spread worldwide. The virus originated from a marketplace in Wuhan where there was human exposure to poultry, snakes, bats and other farm animals.
A study claims that the virus is a recombinant virus, or two strains of a virus combined to create another virus. In this case, the coronavirus is a hybrid between a bat-origin coronavirus and an unknown-origin virus.
Infected areas
According to WHO, as of March 3, there are 90,870 confirmed global cases of the coronavirus. The Centers for Disease Control and Prevention states that there are 2,462 confirmed deaths from the virus.
The nations highlighted in blue have cases of the virus present.
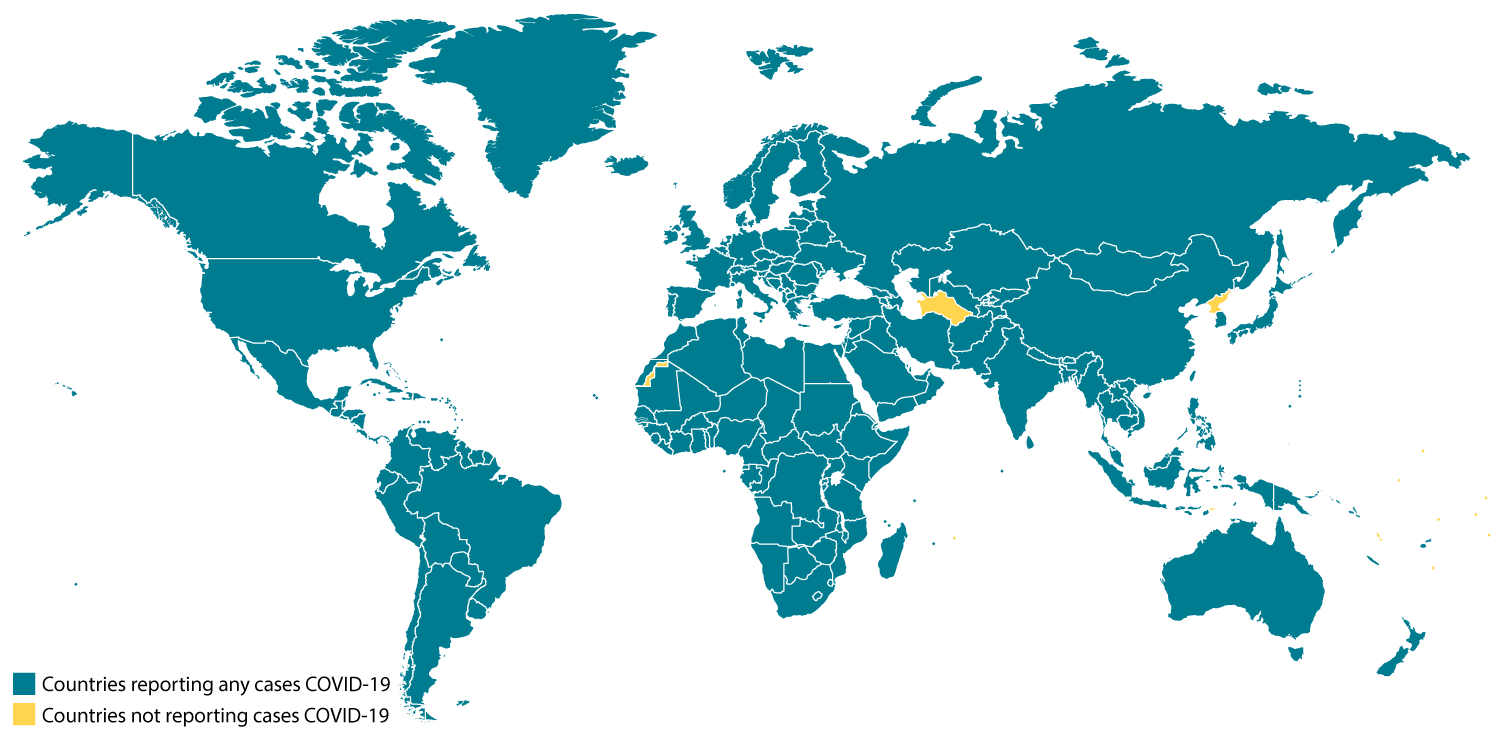
As of March 4, there are 33 confirmed cases of the virus in Canada. The majority of the cases, 20, are in Ontario. The federal government said in a COVID-19 outbreak update that travelling risk for Canadians is generally low, but that it varies depending on the country Canadians are travelling to and from. The spread of COVID-19 in other countries is being closely monitored by the Public Health Agency of Canada.
Vaccine development
Scientists and pharmaceutical companies are working fast to create a vaccine for COVID-19. However, the timeframe for vaccine development can vary between a year and 18 months. Drug companies Inovio Pharmaceuticals Inc. and Moderna are working towards a vaccine.
One way vaccines are developed is that copies of a virus are made, specifically the parts that infiltrate cells, and a person is exposed to these copies. As a response, the person’s body creates antibodies to the virus. Through this process, the individual gains immunity to the virus if they were exposed to it in their everyday interactions.
As early as this month, Moderna will be holding a trial for its vaccine’s safety with 45 healthy individuals. It will take six to eight months of trials on a larger group to determine whether the vaccine can successfully immunize people. After all this, the vaccine will need to be manufactured at a larger scale.

